Emerging therapy for HFpEF patients
- | By Ultromics
- Articles, Heart Failure
Recent clinical trials investigating sodium-glucose cotransporter 2 inhibitors (SGLT2i) have highlighted that this drug is highly effective in treating patients with heart failure with preserved ejection fraction (HFpEF).
HFpEF is a complex disease which accounts for more than half of all heart failure (HF) hospital admissions and is an increasing disease burden. [1] The prevalence of HFpEF is climbing, reflecting an increasingly elderly and comorbid population, as well as reinforcing the need for more effective therapies.[2]
SGLT2is are a class of anti-diabetic drugs that have demonstrated large cardiovascular benefit in both diabetic and non-diabetic, acute and chronic heart failure patients. They recently gained a new role in the management of heart failure with reduced ejection fraction (HFrEF), and now they are the first drug class to improve cardiovascular outcomes in HFpEF.
Specifically, Jardiance (empagliflozin) was approved for use by the FDA in February 2022[4], following the results of the EMPEROR-Preserved study which demonstrated a 21% lower relative risk of hospitalizations for HFpEF patients taking empagliflozin.[3]
More recently, the DELIVER Phase III results demonstrated Farxiga's (dapagliflozin) efficacy in heart failure, which provided further evidence of support for SGLT2 inhibitors.[4]
Additionally, the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Failure Society of America (HFSA) recommend broader use of SGLT2is in clinical practice and earlier initiation of guideline-directed medical therapy.[5]
This article looks at the therapeutic potential for HFpEF patients and summarizes the results from the EMPEROR-Preserved and DELIVER trials.
Current Treatment Strategies in HFpEF
Despite an influx of pathophysiology studies and outcome trials that are reshaping our understanding of HFpEF as a complex, multi-systemic disease, the inconclusive benefits of available treatment options for HFpEF remain a burden.
Angiotensin-converting enzyme (ACE) inhibitors (± neprilysin inhibitor), beta blockers, and mineralocorticoid receptor antagonists have been the cornerstone of treatment of HFrEF,[8] but unfortunately, unlike HFrEF, there are no treatments for HFpEF to reduce morbidity and mortality[9,10,11], despite the worrying trend of increasing prevalence of this condition.
Treatment, therefore, focuses on symptomatic management of fluid overload, rate control of atrial fibrillation, and blood pressure management. Treatment should be individually based, with treatment focusing on underlying comorbidities (this may of course mean patients are on treatments such as ACE inhibitors and beta blockers anyway).[6]
SGLT2 inhibitors were very recently added to both the American and European guidelines for the treatment of HFpEF after EMPEROR-Preserved and DELIVER trials showed reduced risk of cardiovascular death or hospitalization for HF in patients with HFpEF.

.png?width=233&height=131&name=Ultromics%20Blog%20Featured%20Image%201600%20%C3%97%20900%20(1).png) |
Related read: Learn about the challenges for diagnosing HFpEF. |

What are SGLT2is?
SGLT2is are a relatively novel class of glucose-lowering drug, originally utilized as anti-diabetic drugs that lower blood glucose levels in patients with type 2 diabetes mellitus (T2DM).
In diabetes, SGLT2is primarily work by inhibiting glucose reabsorption at the renal proximal tubule. Other effects of these medications include increasing diuresis and natriuresis, lowering blood pressure, stimulating erythropoiesis, improving cardiac energy metabolism, reducing inflammation, inhibiting the sympathetic nervous system, preventing cardiac remodeling, preventing ischemia-reperfusion injury, inhibiting the Na+/H+ exchanger, reducing hyperuricemia, increasing autophagy and lysosomal degradation, decreasing epicardial fat, increasing erythropoietin levels, increasing circulating vascular progenitor cells, decreasing oxidative stress, and improving vascular function.[7]
The earliest clinical trial investing therapeutic effects of SGLT2i (empagliflozin) in type 2 diabetes patients has shown that the drug is highly effective in reducing myocardial infarction, stroke, heart failure-related hospitalization, and cardiovascular death. Over the last years, we have witnessed the inclusion of the use of SGLT2is for the treatment of patients with heart failure.

Currently, four SGLT2is (empagliflozin, dapagliflozin, canagliflozin, and ertugliflozin) are licensed by the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA).
Empagliflozin in HFpEF (EMPEROR-Preserved)
The EMPEROR-Preserved trial, released in 2021, is the first randomized controlled trial testing the efficacy and safety of SGLT2is (empagliflozin) in patients with HFpEF. The therapy was able to significantly reduce cardiovascular death or hospitalization in patients with HFpEF. [3]
The randomized, multicenter, double-blinded, placebo-controlled trial set out to evaluate the effects of SGLT2 inhibition with empagliflozin on major heart failure outcomes in patients with HFpEF, looking at the combined occurrence of cardiovascular death or hospitalization as a primary outcome, occurrence of all hospitalizations for HF as a first secondary outcome and the rate of decline in eGFR as a second secondary outcome.
After screening 11,583 patients, the study enrolled 5,988 patients with symptomatic heart failure and preserved ejection fraction (EF > 40%). The patients were randomized in a 1:1 fashion into two groups to receive either empagliflozin 10 mg per day (n = 2,997) or placebo (n = 2,991); in addition to usual therapy. [3]
The patients were followed up with periodically for a median duration of 26.2 months to check symptoms, health status (assessed with the Kansas City Cardiomyopathy Questionnaire), and adverse events. It is noteworthy that about half of these patients were diabetic.
The EMPEROR-Preserved study found that treatment with empagliflozin reduced the occurrence of HHF and cardiovascular death as a combined primary outcome. Specifically, SGLT2 inhibition led to a 21% risk reduction of the composite of cardiovascular death or hospitalization for heart failure, which was mainly related to a 29% lower risk of hospitalization for heart failure rather than effect on cardiovascular death empagliflozin.[3]

SGLT2 inhibition led to a 21% risk reduction of the composite of cardiovascular death or hospitalization for heart failure.
Cardiovascular death and hospitalization were both significantly lower in the empagliflozin group compared to the placebo group (415 patients; 13.8% versus 511 patients 17.1%, hazard ratio, 0.79; 95% CI [0.69–0.90]; P < 0.001). The number of patients treated with empagliflozin needed to prevent one primary outcome event was 31 (95% CI).[3]
Hospitalization for heart failure occurred in 8.6% of the empagliflozin group and 11.8% of the placebo group. However, cardiovascular death numbers were not significantly different (7.3% in the empagliflozin group, versus 8.2% in the placebo group).[3]
Estimated cumulative incidence of the primary outcome (composite of cardiovascular death or hospitalization for HF) in the empagliflozin group compared to the placebo group. [5]
Dapagliflozin in HFpEF (DELIVER)
The DELIVER trial results, presented at ESC Congress 2022 and simultaneously published in the New England Journal of Medicine, add to the growing evidence that SGLT2 inhibitors are beneficial for HFpEF patients. [4]
The study enrolled 6,263 patients with HF and a left ventricular ejection fraction (LVEF) of more than 40% from 350 sites in 20 countries.
Participants were randomly assigned to receive either dapagliflozin (10 mg once daily) or a matching placebo, in addition to usual therapy. The primary outcome was a composite of worsening HF or cardiovascular death, as assessed in a time-to-event analysis. The median follow-up was 2.3 years.
Results found the primary outcome occurred in 512 of the 3,131 patients (16.4%) in the dapagliflozin group and in 610 of the 3,132 patients (19.5%) in the placebo group. Researchers observed worsening HF in 368 patients (11.8%) in the dapagliflozin group and 455 patients (14.5%) in the placebo group. Cardiovascular death occurred in 231 patients (7.4%) in the dapagliflozin group and 261 patients (8.3%) in the placebo group.[4]
In other findings, total events and symptom burden were lower in the dapagliflozin group. In addition, researchers noted that overall results were consistent across prespecified subgroups, including those defined according to LVEF and those with or without diabetes.
Estimated cumulative incidence of the primary outcome (composite of worsening HF or cardiovascular death) in the dapagliflozin group compared to the placebo group. [6]
Early and Precise Detection is Key
The EMPEROR-Preserved and DELIVER trials are large landmark trials with similar designs that provide compelling evidence of the benefit of using empagliflozin and dapagliflozin in patients with HFpEF. It is a major step forward for reducing mortality rates in this vulnerable population and will inform future guidelines for their broader use in clinical practice.
In the 2022 Guideline for the Management of Heart Failure from The American College of Cardiology (ACC), American Heart Association (AHA), and Heart Failure Society of America (HSFA), SGLT2 inhibitors were first put forward and given a 2a class recommendation for the treatments of in HFpEF patients. [8]
To further support these emerging therapies, precision detection of HFpEF is key.
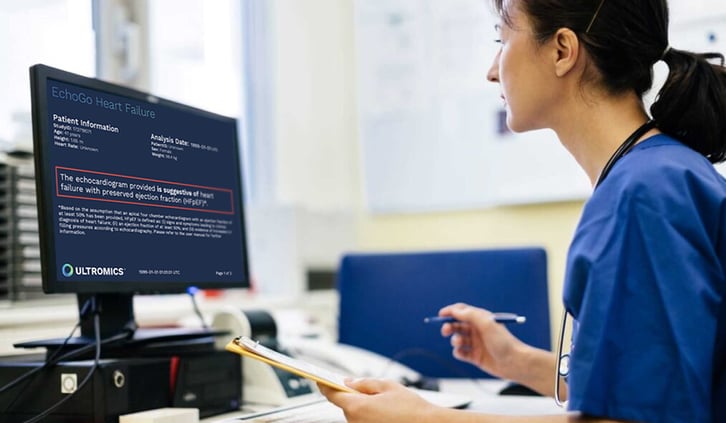
Recent research has found that the AI in EchoGo Heart Failure has demonstrated a 25% increase in diagnostic accuracy from current clinical practice in the detection of HFpEF.
The novel, FDA-cleared platform that applies AI to echocardiography to simplify the detection of HFpEF, a diagnosis that can be challenging to make, to allow more expeditious treatment of emerging new therapies, such as with SGLT2is, to improve quality of life.
References:
- Heath R, Johnsen H, Strain WD et al. Emerging Horizons in Heart Failure with Preserved Ejection Fraction: The Role of SGLT2 Inhibitors. Diabetes Therapy. 2022;13:241-250
- Anker SD, Butler J, Filippatos G, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. New England Journal of Medicine 2021;385:1451-1461 AstraZeneca. Farxiga-Improved Symptom Burden and Health-Related Quality. 2022
- AstraZeneca. Farxiga-Improved Symptom Burden and Health-Related Quality. 2022
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2022;79:263-421
- Heath R, Johnsen H, Strain WD et al. Emerging Horizons in Heart Failure with Preserved Ejection Fraction: The Role of SGLT2 Inhibitors. Diabetes Therapy. 2022;13:241-250
- Issa VS. Is There Room for New Drugs in the Treatment of Advanced Heart Failure: SGLT2i? ABC Heart Fail Cardiomyop [Internet]. 2022;2(2):195–7.
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–3726.
Curious about upcoming research and innovation?
Sign up to hear about the latest news.