
AI enabled global longitudinal strain quantification in hospitalized COVID-19 patients with myocardial injury.
- | By Ultromics
William Hawkes, Katherine Tilkes, Halley Davison, Christopher G. Scott, Hania Piotrowska, William Hansen, Jeremy Thaden, Gary M. Woodward, Patricia A. Pellikka.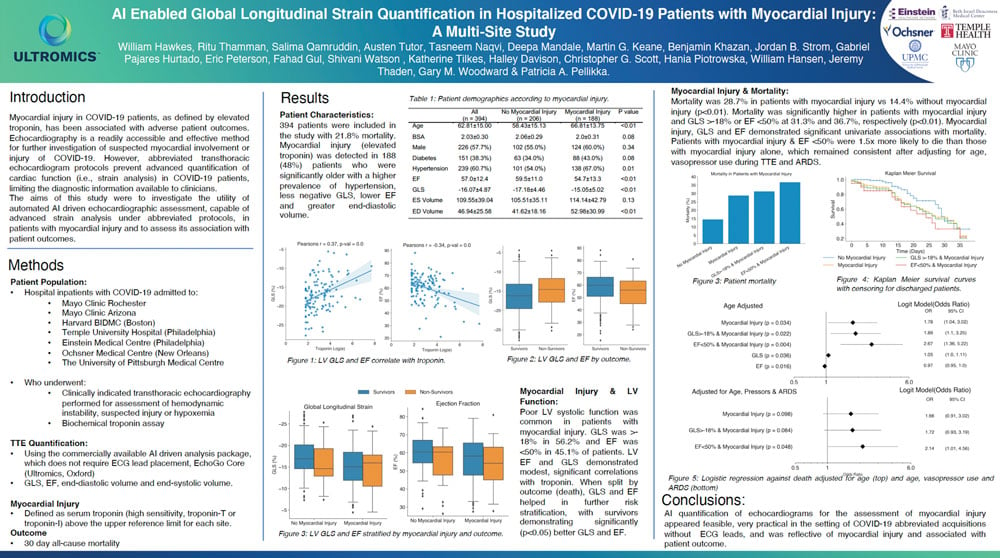
Poster of the study. Click image to open in new window.
Background
Emerging evidence suggests that COVID-19 disease severity and patient outcomes are associated with myocardial injury. Echocardiography is an accessible, cheap and effective method for further investigation of suspected myocardial involvement or injury. Abbreviated transthoracic echocardiogram protocols prevent advanced quantification of cardiac function (i.e. strain analysis) in COVID-19 patients, limiting the diagnostic information available to clinicians. The aim of this study was to investigate the utility of Automated AI driven echocardiographic assessment, capable of advanced strain analysis under abbreviated protocols, in patients with myocardial injury and assess its association with patient outcomes.
Methods
77 consecutive patients hospitalised with confirmed COVID-19 who underwent clinically indicated echocardiographic assessment were analysed using the AI platform, EchoGo Core (Ultromics Ltd, Oxford, UK). Left ventricular global longitudinal strain, ejection fraction (biplane), end diastolic and end systolic volume was assessed. Myocardial injury was defined as high sensitivity troponin-T being above the upper reference limit. Univariate and multivariate logistic regression was used to evaluate the association between patient outcomes (prolonged hospitalisation or death) and echocardiographic metrics, clinical data and the presence of myocardial injury.
Results
Troponin defined myocardial injury was present in 39 patients (51%). Patients with myocardial injury were older (53±15 years vs 67±16 years), had an increased prevalence of diabetes (21% vs 49%) and made up 65% of the cases with poor outcomes of prolonged hospitalization (>21 days) or death. Age adjusted univariate analysis demonstrated a significant association between myocardial injury and adverse outcomes (Odds Ratio: 2.36, 95% confidence intervals: 1.69, 8.03). Patients with myocardial injury and abnormal global longitudinal strain had a greater association with poor outcomes (Odds Ratio: 4.64, 95% confidence intervals: 1.55, 13.88) which remained consistent after multivariate analyses adjusting for severe disease, acute kidney injury, chronic kidney disease and organ failure.
Conclusion
We present the first evidence that fully automated, AI enabled, strain analysis of patients hospitalized with COVID-19 is clinically informative in patients demonstrating serological evidence of myocardial injury echocardiograms that completely eliminates inter-operator variability on image analysis.