Ultromics receives FDA clearance for its breakthrough device for HFpEF detection
- | By Ultromics
- Press Release
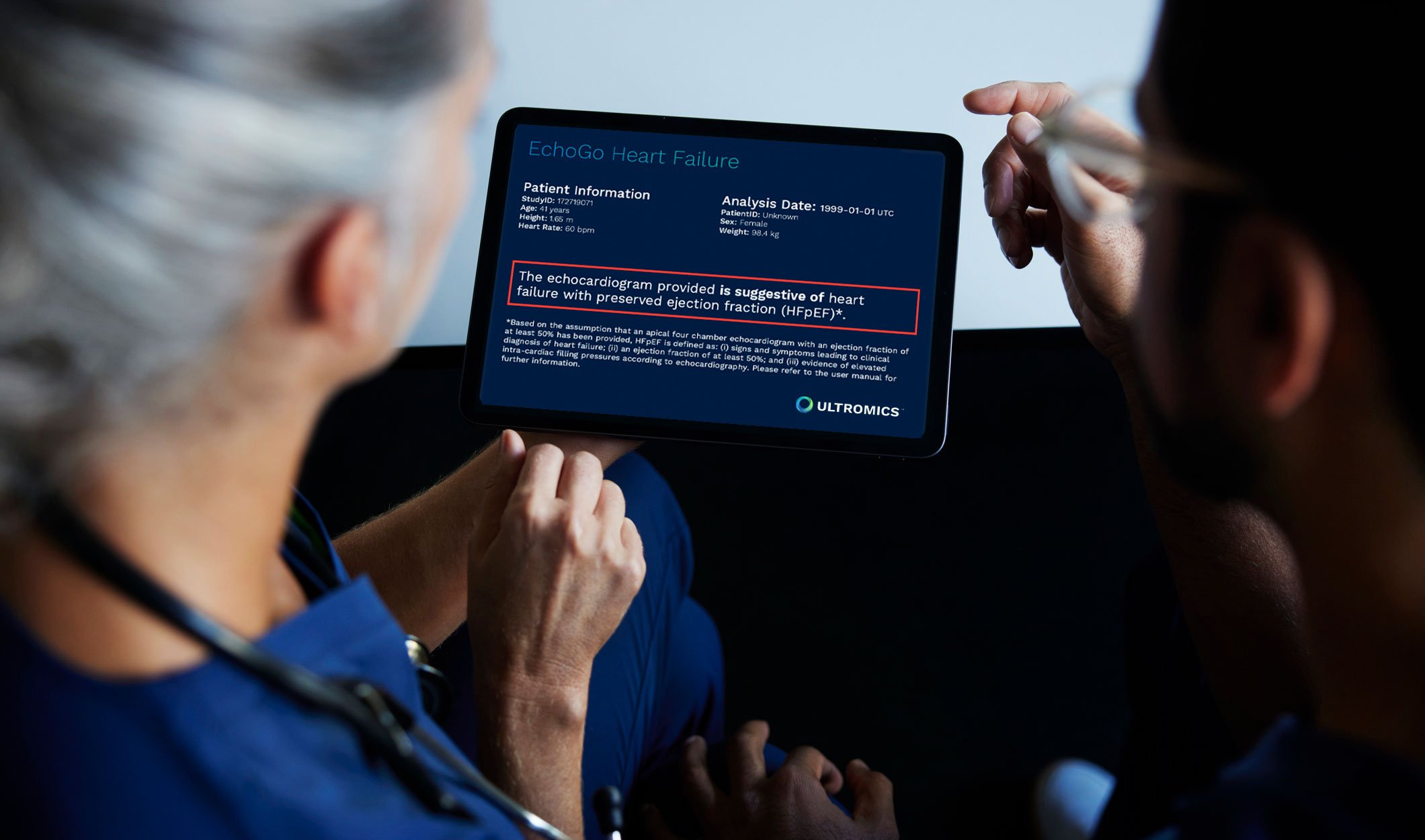
EchoGo® Heart Failure is an AI-based platform that enables precision detection of heart failure with preserved ejection fraction(HFpEF). EchoGo® Heart Failure revolutionizes the detection of HFpEF – the biggest unmet need in cardiovascular medicine1
Oxford, UK, December 6th, 2022: Ultromics’ EchoGo® Heart Failure, an AI solution for echocardiography with the potential to revolutionize the diagnosis of heart failure with preserved ejection fraction (HFpEF), has received US Food and Drug Administration (FDA) clearance. The news puts EchoGo® Heart Failure in the 7% of devices that have gone on to obtain full marketing authorization after being awarded FDA breakthrough status2.
The clinical and technological breakthrough was developed by echocardiography and AI experts from Ultromics, a spin-out of the UK’s University of Oxford, in collaboration with Mayo Clinic. The device uses AI to accurately detect HFpEF from a single echocardiogram image, which accounts for 50% of the 64 million cases of heart failure worldwide and has overtaken heart failure with reduced ejection fraction (HFrEF) as the most prevalent form of the deadly disease3.
This development marks a huge leap forward from traditional diagnostic algorithms for HFpEF, a heterogeneous syndrome that can be challenging to identify, and is missed in up to 75% of cases4. Current approaches include time-consuming and often inconclusive diastolic function assessment, and require a highly specialized, increasingly rare skillset, and often invasive testing. To counter this, EchoGo® Heart Failure has a vital role to play in the future HFpEF landscape.
The FDA clearance comes just weeks after Ultromics demonstrated its commitment to addressing this area of significant unmet medical need by joining the FNIH (Foundation for the National Institutes of Health) Accelerating Medicines Partnership Heart Failure (AMP HF®) program. The $37 million, five-year multi-stakeholder collaboration, managed by FNIH, is a collaboration between the National Institutes of Health (NIH) and the National Heart Lung and Blood Institute (NHLBI), the FDA, the American Heart Association (AHA), the American Society of Echocardiography, and industry members. The partnership seeks to develop a deeper understanding of HFpEF and develop more precise strategies and targeted therapies that could improve the lives of millions and improve survival while minimizing exposure to invasive techniques.
There is an urgent need to develop predictive tools to help diagnose HFpEF patients. Patients can now benefit from new therapy drugs, such as SGLT2is, which has been shown to significantly reduce both hospitalizations and potentially fatal adverse events. The simultaneous clearances of EchoGo® Heart Failure to improve HFpEF detection and SGLT2 to improve treatment represents a giant leap forward in addressing the biggest unmet need in cardiovascular medicine.
Dr Ross Upton, CEO and Founder of Ultromics, said: “We are delighted that the FDA has recognized EchoGo® Heart Failure as a breakthrough device and has cleared the technology to provide reliable detection of HFpEF. The technology improves the accuracy of HFpEF detection, enabling more patients to receive treatment which will reduce the significant burden on patients and healthcare systems alike.
“Although compelling progress has been made in the diagnosis and treatment of many forms of heart disease, heart failure hospitalizations and mortality continue to rise globally. It is now time to make a change. Together with our FNIH AMP HF partners, we aim to redefine the heart failure care pathway and improve world-wide patient outcomes.”
Patricia A. Pellikka, MD, Vice Chair, Department of Cardiovascular Medicine at Mayo Clinic, said “It has been a pleasure to collaborate with the team at Ultromics to develop and test EchoGo® Heart Failure. This novel solution applies AI to cardiovascular imaging to greatly simplify the identification of patients with HFpEF, a diagnosis that can be challenging to make, and allow more expeditious treatment. HFpEF currently is associated with high rates of hospitalization and mortality. By facilitating early diagnosis and treatment, we can improve the lives of many.”
Dr Julie Gerberding, Chief Executive Officer at the FNIH, said: “The Foundation for the National Institutes of Health will harness the valuable perspectives and expertise of a select number of collaborations, including Ultromics, to alleviate this unmet need and pave the way for better classification and more precise treatment strategies.”
What is HFpEF?
HFpEF is a type of heart failure often associated with co-morbidities and tends to be caused by increased pressure within the chambers of the heart. The ejection fraction, or the volume of blood ejected from the left ventricle at each heartbeat, however, remains in normal ranges. This makes it exceedingly difficult to detect using traditional diagnostics, which can miss up to 75% of cases4.
The symptoms, which include shortness of breath, chest discomfort, and debilitating fatigue, can have an enormous impact on a person’s quality of life. It is a leading cause of hospitalizations and is often deadly, carrying a five-year survival rate of just 35% to 40%5.
Historically, there has been no effective treatment for HFpEF. However, a new therapy, sodium-glucose cotransporter 2 inhibitors (SGLT2is), which has demonstrated a relative risk reduction in heart failure hospitalizations by 29%6, has recently been approved for use. It places an even greater emphasis on the need for precise diagnosis of HFpEF.
What is EchoGo® Heart Failure?
Echocardiography is the most widely used and highly valued cardiac imaging procedure. It provides rapid results and is portable, safe, and more cost-effective than other imaging modalities. However, existing tools and measurement packages have limitations.
Evaluating the presence or risk of HFpEF is extremely variable in current clinical practice. The average sensitivity and specificity to distinguish HFpEF is quite poor, estimated to be 74% and 65% respectively, with data taken from 9 key publications”7-15.
These high missed diagnosis rates and current tools generally stop short of linking echocardiography findings to treatment interventions and patient pathways. Importantly, traditional echocardiography suffers from variability across all phases including image acquisition, measurement, and interpretation.
Ultromics harnesses the power of AI and takes HFpEF detection to the next level. The company strives to improve patient outcomes by enabling screening, precision diagnosis, and deep phenotyping of HFpEF that directly maps to treatment pathways.
EchoGo® Heart Failure aims to prevent HF hospitalizations and reduce mortality through better detection of HFpEF and is therefore an integral part of that mission. Built-in collaboration with the Mayo Clinic, this solution analyzes millions of pixels within a single echocardiogram to deliver precision detection of HFpEF.
EchoGo® Heart Failure has demonstrated:16
- 90% accuracy in detecting HFpEF in the validation dataset;
- 87.8 Sensitivity and 83% Specificity in the independent testing dataset;
- 68% more HFpEF patients correctly identified vs. clinical algorithms in the independent testing dataset.
HFpEF is a significant burden, and the solution needs to start with an accurate diagnosis. Up until now, we have lacked a gold standard, easy-to-use approach. But the FDA-cleared EchoGo® Heart Failure can help combat this commonly missed disease. The platform is the first HFpEF detection algorithm that will help support diagnosis and patient selection for therapy, ultimately improving quality of life and reducing the significant burden HFpEF has on healthcare.
For more information visit here.
Mayo Clinic has a financial interest in the technology referenced in this press release. Mayo Clinic will use any revenue it receives to support its not-for-profit mission in patient care, education and research.
References:
- Shah JS, Butler J, Shah SH, et al. Accelerating therapeutic discoveries of heart failure: a new public-private partnership. Nature Reviews Drug Discovery. 2022;21:781-782
- Eisenhart S. FDA’s breakthrough medical device designations tally nears 700. Emergo Group. 2022 [Accessed 2023] Savarese G and Lund LH. Global public health burden of heart failure. Cardiac Failure Review. 2017;3:1:7-11.
- Kapłon‐Cieślicka A, Laroche C, Crespo-Leiro MG et al. Is heart failure misdiagnosed in hospitalized patients with preserved ejection fraction? From the European Society of Cardiology‐Heart Failure Association EURObservational Research Programme Heart Failure Long‐Term Registry. ESC heart failure. 2020;7:2098-2112.
- Oktay AA, Rich JD, & Shah SJ. The emerging epidemic of heart failure with preserved ejection fraction. Current Heart Failure Reports, 2013;10:401-410.
- Anker SD, Butler J, Filippatos G, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. New England Journal of Medicine 2021;385:1451-1461 L ncellotti P, Galderisi M, Edvardsen T, et al. Echo-Doppler estimation of left ventricular filling pressure: results of the multicentre EACVI Euro-Filling study. European Heart Journal of Cardiovascular Imaging. 2017;180:961-8
- Obokata M, Kane GC, Reddy YNV, et al. Role of Diastolic Stress Testing in the Evaluation for Heart Failure With Preserved Ejection Fraction: A Simultaneous Invasive-Echocardiographic Study. Circulation. 2017;1359:825-38.
- Misun Pak M, Takeshi Kitai MP, Atsushi Kobori MP, et al. Diagnostic Accuracy of an Integrated Echocardiographic Algorithm to Estimate Left Ventricular Filling Pressure. Cardiovascular Imaging. 2022;6
- Van de Bovenkamp AA, Enait V, S de Man F, et al. Validation of the 2016 ASE/EACVI Guideline for Diastolic Dysfunction in Patients With Unexplained Dyspnea and a Preserved Left Ventricular Ejection Fraction. Journal of the American Heart Association. 2021;10:e021165
- Van de Bovenkamp AA, Wijkstra N, Oosterveer FPT, et al. The Value of Passive Leg Raise during Right Heart Catheterization in Diagnosing Heart Failure with Preserved Ejection Fraction. Circulation Heart Failure. 2022;15:e008935.
- Verbrugge FH, Reddy YNV, Sorimachi H, et al. Diagnostic scores predict morbidity and mortality in patients hospitalized for heart failure with preserved ejection fraction. European Journal of Heart Failure. 2021;23:954-63.
- Nielsen OW, Valeur N, Sajadieh A, Fabricius-Bjerre A, Carlsen CM, Kober L. Echocardiographic subtypes of heart failure in consecutive hospitalised patients with dyspnoea. Open Heart. 2019;6(1).
- Nikorowitsch J, Bei der Kellen R, Kirchhof P, et al. Applying the ESC 2016, H 2 FPEF, and HFA-PEFF diagnostic algorithms for heart failure with preserved ejection fraction to the general population. ESC Heart Fail. 2021;85:3603–12.
- Sanders-van Wijk S, Aizpurua AB, Brunner-La Rocca HP, et al. The HFA-PEFF and H2FPEF scores largely disagree in classifying patients with suspected heart failure with preserved ejection fraction. European Journal of Heart Failure. 2021;23:838-840
- EchoGo Heart Failure FDA Submission
Curious about upcoming research and innovation?
Sign up to hear about the latest news.

