Putting AI-Powered EchoGo® Devices into Practice at City of Hope Comprehensive Cancer Center
- | By Ultromics
- Dr. Faizi Jamal
In a recent interview, Dr. Faizi Jamal reflected on his experience implementing EchoGo® Heart Failure and EchoGo® Amyloidosis within the clinical workflow at City of Hope National Medical Center. He highlights the motivations behind early adoption, the value of EchoGo® insights, and how the technology is helping clinicians identify cardiac amyloidosis in an enriched HFpEF population.
Key points:
- EchoGo® provides actionable insights, improving care for patients
- Integrating AI helps pinpoint which HFpEF patients are most likely to have underlying amyloidosis and who should be referred for confirmatory testing
- Implementation success requires alignment and a team approach

Q1. What were some of your initial goals in implementing AI at City of Hope?
When I joined City of Hope in 2017, my goal was to ensure that our evaluations of cardiac function were accurate and reliable. Echocardiography has traditionally been more of an art than a science, with variability in image acquisition, machines, and physician interpretation.
To address this issue, we developed standardized protocols for how echocardiograms would be performed and how function would be reported, but we still saw persistent differences in ejection fraction (EF). Nationally, up to a 10% variation between readers is considered acceptable, yet that same threshold defines cardiotoxicity, which can determine whether a patient receives or is withheld treatment.
We needed an objective method to reduce variability and measure EF consistently. Artificial intelligence was a natural solution, and Ultromics emerged as a frontrunner in this space.
Q2. Have EchoGo® Heart Failure and EchoGo® Amyloidosis helped achieve those goals?
Initially, we used EchoGo® to improve core measurements such as EF and global longitudinal strain. Since then, it has advanced toward disease identification, which has been eye-opening. When we first started, we were simply asking whether AI could deliver accurate, reproducible measurements. We never imagined that it would also help identify conditions like heart failure or amyloidosis, and that shift has allowed us to achieve more than we originally set out to do.
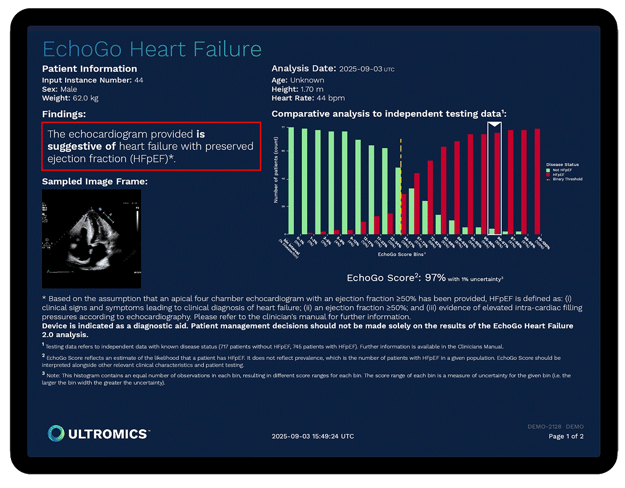
EchoGo® Heart Failure has given our faculty confidence to take echo findings one step further by drawing a clear conclusion, stating, for example, that the patient has heart failure with preserved ejection fraction (HFpEF) rather than just listing elevated pressures.
That clarity has made our reports far more actionable. Referring physicians now have something concrete to act on, which often means calling patients back to the clinic, referring them to cardiology, or initiating management strategies. When I say care has improved as a result, that’s what I mean—we are providing information that prompts people to intervene.
Q3. What are your thoughts on the EchoGo® score?
The EchoGo® score has been immensely helpful, especially when findings are less clear with parameters borderline or inconsistent. In those cases, having the EchoGo® score helps us determine whether the study aligns with patients who definitively have heart failure.
City of Hope now incorporates the EchoGo® score into every report. It gives ordering clinicians a clearer sense of urgency in how to manage their patients. Alongside the AI finding, we state the method used and the associated likelihood. For referring physicians, that number provides important context. A 51% score suggests caution and closer follow-up, whereas a 99% or even 100% score signals there is little doubt the patient has heart failure and intervention is needed.
Q4. Why is the ability to screen for cardiac amyloidosis important?
Cardiac amyloidosis is notoriously difficult to diagnose, and the need for earlier detection is critical. Roughly 15% of patients with HFpEF and about 16% of those with aortic stenosis have transthyretin amyloidosis (ATTR), a condition that is now treatable with therapies that can slow or even arrest disease progression.
The clinical signs are often nonspecific, and by the time changes appear on an echocardiogram, years of amyloid deposition have already occurred. Even at academic centers, where we are attuned to subtle findings, the disease is often recognized late. Across the broader medical community, millions of echocardiograms are performed each year, and nuanced signs of amyloidosis can be easily overlooked. Having AI act as an “over-reader” provides an additional layer of support, flagging cases that human eyes might miss.
Q5. How has EchoGo® Amyloidosis changed your diagnostic approach?
Before using EchoGo® Amyloidosis, we relied on our most experienced readers to detect subtle clues like mild wall thickening, reductions in strain, or an apical sparing pattern. Early cases were nearly impossible to identify with confidence, and at best, we would recommend further evaluation for infiltrative disease. Now, when the algorithm categorizes a study as suggestive of amyloidosis, we have more information to act on. I’ve had colleagues refer patients after the AI flagged a study that initially showed no obvious signs, and on review I identified multiple concerning features.
By improving sensitivity and specificity, AI has the potential to bridge the gap between a broad diagnosis of HFpEF and the costly or invasive tests used to confirm amyloidosis, such as cardiac MRI, nuclear scans, or biopsy. AI is a conglomerate of the best of us—providing that level of expertise consistently in every read—and by doing so, it improves diagnosis and helps identify more patients who may benefit from treatment.
Q6. What advice would you give to other centers considering implementing an AI solution like EchoGo® Heart Failure?
The key is to be open to change and persistent in your objective to enhance patient care. Progress doesn’t happen without change, and success will come as the entire group begins to see where AI tools like EchoGo® can fit into practice.
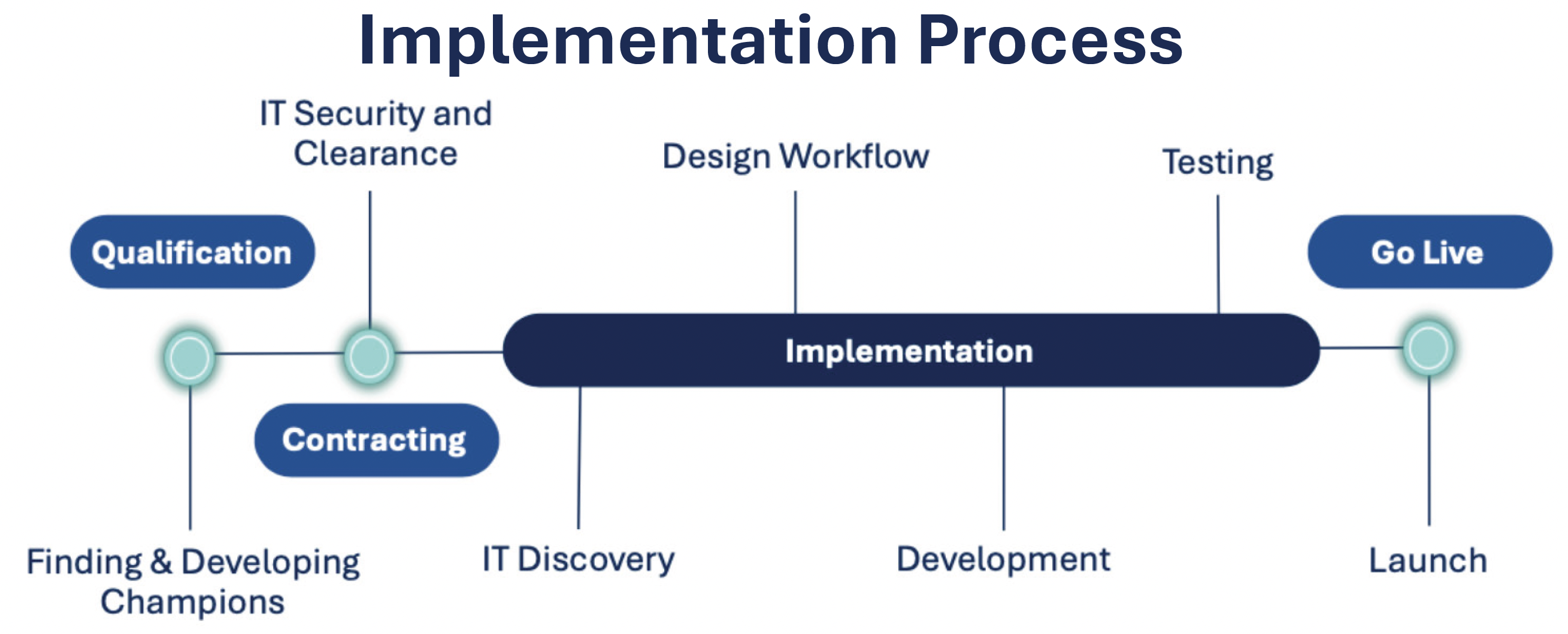
It is also important to plan ahead for how positive AI findings will be managed. We developed a systematic approach, including standardized reporting, EchoGo® scores, and referrals when appropriate, to ensure results translate into better care. Equally important is patience, as successful adoption requires buy-in across the institution and time for teams to adjust to new workflows.
Q7. Are you using other AI tools at City of Hope?
Within cardiology, we’re not currently using any other AI products. In clinic, however, we’ve adopted an AI tool that functions as a scribe, listening to patient encounters and generating a structured history, assessment, and plan. City of Hope is also pioneering its own AI initiatives, which extend to drug discovery, early cancer detection, and deeper insights into cancer evolution and disease progression. One internal product that we use routinely is Hope LLM, our own generative AI platform, which removes the administrative burden of new patient onboarding, matches patients to clinical trials, and enables generative AI responses that are personalized to individual patient records.